Cleft Lip & Palate Explained
What effects can a cleft have on my child?
Depending on the severity of the cleft, it may affect:
Appearance
The initial appearance of a facial cleft, even if it is minor, can come as a shock to the family and friends. This initial feeling of upset is normal and you may find it helpful to talk to other parents with similar experiences. The Cleft Lip and Palate Association of Ireland can help you make contact with other parents. Your cleft team will be available to answer any questions you may have.
Feeding
In order to breast or bottle feed, your baby must be able to create good suction inside the mouth and position the tongue properly. This is done by closing the soft palate against the back of the mouth and the lips around the nipple or teat. With a cleft palate, babies will draw in air via the nose when attempting to suck. Some babies have a smaller lower jaw which can make swallowing difficult as they cannot position their tongue properly.
Weaning your child
Your baby should wean in the usual manner. Puréed foods can be introduced around 4 months and mashed foods between 6 and 9 months. Most babies find it easier to feed with semi-solid foods, which are less likely to spill back into the nose and out the nostrils.
Useful website for introducing spoon feeds for your baby:
www.hse.ie (search weaning)
www.bordbia.ie/nutrition/babys-first-year/
www.weaning.ie
Effect on hearing
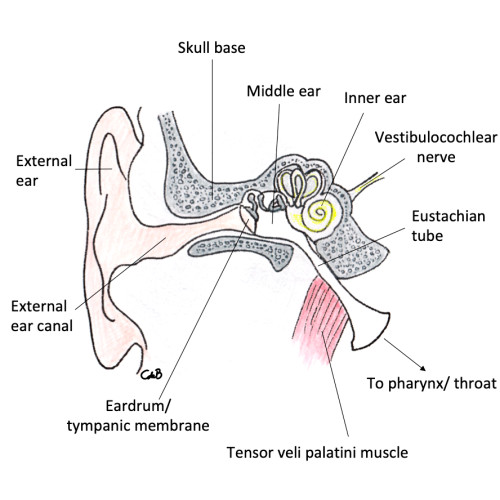
The ear is composed of three parts – the outer ear, the middle ear and the inner ear. Sound striking the eardrum is transmitted via 3 small bones to the inner ear, from where it is conducted to the brain by the auditory nerve.
Hearing can be affected in children with a cleft palate. Normally, the middle ear contains air and is connected to the back of the nose via the Eustachian tube. In a cleft palate, the muscles that open this tube do not work as well as usual, meaning that air cannot enter the middle ear often enough. This can lead to a build-up of negative pressure, resulting in thick fluid collecting in the middle ear and reducing sound transmission to the inner ear.
Every newborn baby has their hearing checked as part of the National Newborn Hearing Screening Programme.
If your child has a cleft palate, it should also be offered a second hearing test by the Community Audiology Services, which ideally takes place 3 months following their palate repair. It is important that your child has this hearing check so that we can be sure they can hear properly and develop their language. If your child has not been offered this follow-up screening, please contact your cleft team, who will be able to help. If any concerns are raised at these appointments, management options will be discussed and agreed.
Following discharge from Community Audiology, children with a cleft palate should normally receive an Audiology Assessment when they are 3 and 5 years of age. If there are concerns about your child’s hearing outside these designated testing ages, the cleft palate team can discuss this with the Audiology Department in your cleft centre.
Effect on Speech
Babies born with a cleft of the palate will automatically get seen by a specialist Speech and Language Therapist (SLT) from the cleft team. Initially, they will help assess your child’s feeding and swallowing, along with the Cleft Nurse Specialist.
A referral will be made to a Community Speech and Language Therapist in your area, who will aim to see your child between 9-12 months of age to assess their communication skills and provide advice on ways to encourage normal speech and language development.
A more detailed speech assessment is carried out at 18 months and 3.5 years of age at your cleft centre. Hearing is also tested again at the cleft centre at age 3.5. If any problems are discovered, your child will be seen with the Plastic Surgeon. It may be necessary for your child to have regular speech and language therapy in the community.
A proportion of children with significant speech problems, despite on-going therapy, will need a specialised assessment of how the palate moves during speech. An assessment in the Palate Investigation Clinic usually involves a whole day and includes a speech assessment and one, or both, of the following special investigations:
A Videofluoroscopy involves talking whilst taking a continuous X-ray, which allows palate movement to be seen from the side.
A Nasendoscopy involves a very small camera looking into the child’s nose to see the palate move from above.
It will help your team to determine whether speech therapy alone, or possibly further surgery, is required to help your child’s speech.
Oral Health
For clefts affecting the lip and upper gum, the overall treatment aim is to provide the child with a normal appearance, smile and dentition by the time they finish growing. In some children, the cleft site involves the upper front teeth and these teeth may be missing or malformed. This can mean there is a particular weakness in this area and special help is needed to keep these teeth healthy.
It is extremely important that the primary (baby) and secondary (adult) teeth do not decay as otherwise it may be impossible to offer orthodontic treatment to get a straight set of adult teeth. Preventing tooth decay is entirely possible by establishing good tooth brushing habits and getting your child used to a healthy diet. The following advice is important:
- Start brushing your baby's teeth as soon as you see their first tooth
- Use a rice-size amount of 1,450ppm toothpaste
(same as adult/older child toothpaste) - Brush at night and at one other time during the day
- Don’t rinse the toothpaste away, just spit it out at the end
- Only give milk or water to drink
- Do not allow your baby to fall asleep with a bottle of milk
- Discontinue bottle use, moving to an open cup around age 1
- Give three main meals and no more than two snacks per day once
- Access primary dental care regularly
Your child should be enrolled with a family dentist or HSE dental service and seen on a regular basis from the age of 12 months, in order to keep the mouth and teeth healthy. You have a very important role in bringing your child to these regular visits and in taking on board the dentist’s advice on diet and oral care.
Orthodontic Treatment
Your child will first meet the Orthodontist when they are 5-7 years of age. Impressions of the gum and teeth are made to help plan future treatment. For some children, simple orthodontic treatment with braces is all that is required to straighten their teeth. Good dental hygiene is necessary for this, as otherwise braces will worsen dental decay, giving a poor outcome.
Children with a single (unilateral) or double (bilateral) cleft affecting the upper dental arch will require bone grafting of the tooth-bearing gums (alveolus), in order to allow the canine tooth (“eye tooth”) to erupt. Before this is carried out, the teeth must be brought into correct position, usually with appliances that expand the upper dental arch. The ideal age is usually between the age of 8 to 12 years and depends on the stage of dental development.
Psychological Welfare
People born with Cleft Lip and/or Palate may have a number of concerns and questions that a psychologist can help with, either through talking on the phone, in a clinic or arranging a separate appointment. We can offer you support, advice, counselling and therapy for a variety of reasons. Just because you or your child was born with a cleft, this does not necessarily mean you will encounter difficulties. Don’t feel like you need to have a big problem to come and speak to us. We are also happy to talk about ways of helping people to deal with day-to-day life, to build on strengths and resources to achieve goals, to promote positive self-esteem and confidence, to help prevent potential problems and to support parents in developing coping strategies.
Here is a list of some of the issues a cleft psychologist may be able to work on with you:
For Children
- Preparing for surgery, dental treatment, orthodontics or other treatment or procedures
- Dealing positively with the attitudes of other people
- Discussing your school experience and working together to think of ways of improving this
- Encouraging healthy self-esteem and well-being
- Working with the whole family to improve relationships
- Dealing constructively with other people’s behaviour, including comments and questions
- Dealing with teasing and bullying
- Helping you to feel confident in your appearance
- Improving ways of communicating
- Preparing for change, such as moving school
- Developing and practising positive ways of thinking
- Talking about some of the things that bother you and finding ways to help
For Parents
- Adjusting to a diagnosis
- Building a positive relationship with your child
- Promoting confidence in you and your child
- Preparing for surgery
- Discussing how to talk to your child about their cleft and what to say to brothers, sisters, family and friends
- Positive strategies for dealing with other people’s reactions
- Support when there is a diagnosis of a genetic condition
- Developing parenting strategies e.g. for encouraging your child to sleep or feed
- Developing ways to support your child, for example when coming into hospital
- Coping with your own worries and anxieties
- Working with the whole family to improve relationships
- Discussing possible solutions to concerns
- Supporting acceptance and adjustment